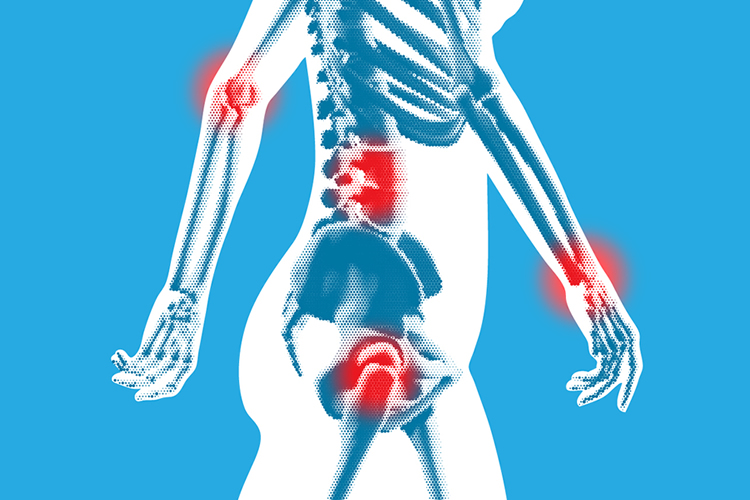
Musculoskeletal injuries resulting from overexertion among healthcare workers are reaching sky-high levels and according to the Bureau of Labor Statistics (BLS), this silent epidemic is affecting nurses and support staff the most within the healthcare industry. While the biggest risk factor for overexertion is manual patient handling, the aging workforce and rising obesity rates likely contribute to the overall problem. In an effort to help break the silence and bring to light such an important issue, we asked 12 safe patient handling and ergonomics experts questions on this very subject.
Thank you to all of the experts who participated in this roundup!
Question #1: What risk factors influence spine stress during patient lifting and handling, ultimately contributing to back pain?
Manon Labreche, PT, CEAS II | Injury Prevention Coordinator, Tampa General Hospital
“Back pain in healthcare workers is repetitive over time. Frequent bending, lifting and twisting places the spine in awkward positions; it can be a challenge to keep the spine in neutral, as handling patients is not the same thing as handling objects. You can’t always keep them close to you, they are unpredictable, their status can change quickly due to pain and unstable vitals, etc. Repositioning in bed and transfers in/out of bed I feel are the highest risk tasks which place healthcare workers at risk of injuries.”
William Marras, Ph.D., CPE | Executive Director & Scientific Director, Spine Research Institute at the Ohio State University
“Risk factors include lifting in and out of bed, chairs and commode. Pushing and pulling of floor-based patient handling equipment; placing slings around patients. Repositioning and transferring, time constraints, and psychosocial pressures in the workplace.”
Arun Garg, Ph.D., CPE, CSPHP | Director, Center for Ergonomics at the University of Wisconsin-Milwaukee
“Manual lifting and transferring including patient weight, ability to cooperate, unpredictability, combativeness, etc.”
Guy Fragala, Ph.D., PE, CSP, CSPHP | Senior Advisor for Ergonomics, Patient Safety Center of Inquiry
“The primary occupational risk factors involved with patient handling activities that influence spine stress are force, repetition, and posture.”
Kermit Davis, Ph.D. | Graduate Program Director for Environmental and Occupational Hygiene Program, University of Cincinnati
“There are many factors that contribute to the stress on the spine, specifically spine loads. A minimal list would include: body weight of patient (obesity is a huge factor), body weight of nurse (lifting upper body when handling patient), body posture of nurse (e.g. depends on technique), mental stress (increased stress increases loads but no one has looked at it in healthcare setting), speed of lift/transfer, and amount of help (or lack of help) from patient. The loads on the spine would be very complex. Further, patient handling is only part of the equation as nurses will handle many other items such as medical devices and in-room furniture. We completed a recent study to document all the handling activities performed by nurses. The results showed that repositioning patients was most performed handling activity but handling medical devices and furniture occur regularly.”
James Collins, Ph.D., MSME | Branch Chief, Analysis and Field Evaluations Branch, Division of Safety Research (DSR), National Institute for Occupational Safety and Health (NIOSH)
“Patient weight far exceeds safe lifting capacities of caregivers, caregivers must assume awkward postures while lifting and moving patients, and caregivers must twist their upper body while lifting.”
Traci Galinsky, Ph.D. | CAPT, U.S. Public Health Service, National Institute for Occupational Safety and Health (NIOSH)
“Manually lifting and handling a patient is itself a major risk factor for spine stress and other musculoskeletal injuries and symptoms, particularly back pain. Manual patient handling includes independent risk factors such as excessive force and awkward postures, whose combined influence increases injury risk even more.”
Heather Monaghan, MHSc, RN | President/CEO, Visioning HealthCare Inc.
“The everyday activities any nurse or nursing assistant performs during their working day. Boosting a patient in bed, turning patients in bed, transferring them from bed to chair or commode, mobilizing a patient to the bathroom. All are high-risk tasks in their own right, but performing them repetitively causes back pain, unseen damage, and for some, career ending injury.”
Suzy Harrington, DNP, RN, MCHES | Chief Wellness Officer, Oklahoma State University
“The twisting and turning movements while lifting, the position of the handler, length of time holding, and especially any weight over 35 pounds.”
Ninica Howard, MSc | Senior Occupational Health and Safety Researcher, SHARP Program at the Washington Department of Labor and Industries
“There are many factors that may contribute to physical stressors placed on nursing staff when handling patients. The growing obesity problem in our society means that nursing staff are handling heavier and heavier patients. In addition, these patients are often sicker, with multiple health issues that may make handling the patient more difficult. The nursing population in the US is generally an older population (approximately 47 years old) meaning that these workers are dealing with age-related issues, such as loss of strength and the cumulative effect of a long work history of handling patients.”
Nancy Hughes, MHA, BSN, RN | Board Member, American Association of Safe Patient Handling and Movement
“Human capacity being exceeded with loads above the NIOSH health care limits; biometrical forces on the spine.”
Question #2: Will the use of machines and other equipment to safely lift and move patients ever completely replace body mechanics?
Manon Labreche, PT, CEAS II | Injury Prevention Coordinator, Tampa General Hospital
“I hope lifting equipment will be used as a standard in all hospitals; however, one must use correct body mechanics while utilizing equipment in order to avoid repetitive strain on the spine. For example, when using equipment, we still want staff to raise the bed at hip level, avoid bending and lifting while applying a sling under a patient, etc., so a combination of equipment and body mechanics is best to help reduce repetitive strain.”
William Marras, Ph.D., CPE | Executive Director & Scientific Director, Spine Research Institute at the Ohio State University
“We need properly designed and available equipment to eliminate the need to manually move patients. The loads on the spine are so large that they make body mechanics ineffective.”
Arun Garg, Ph.D., CPE, CSPHP | Director, Center for Ergonomics at the University of Wisconsin-Milwaukee
“Eventually, yes.”
Guy Fragala, Ph.D., PE, CSP, CSPHP | Senior Advisor for Ergonomics, Patient Safety Center of Inquiry
“It has been determined that demands placed upon the musculoskeletal structure from manual patient handling activities are beyond worker capabilities. Therefore, safe patient handling technology is required. Where patients are not totally dependent, lifting aid devices might be appropriate, which might not totally eliminate the lift but rather reduce risk. Appropriate use of these lifting aid devices is dependent upon a proper patient assessment.”
Kermit Davis, Ph.D. | Graduate Program Director for Environmental and Occupational Hygiene Program, University of Cincinnati
“The use of assist devices is the only way to be safe as there is no way ‘good’ body mechanics can allow you lift a 100+ lb patient (and most exceed 200+) safely. Further, team lifting does not necessarily translate into safe loads on the back as you just don’t divide the weight of the patient by the number of lifters since patients don’t have compliant body weight and team lifting does not translate into equal effort for everyone (i.e. at some level, everyone is working against each other). Nurses are very unique in the fact they are willing to lift such heavy loads. If you were lifting above 30 lb in a manufacturing facility, the line would be shut down. I think lift assist devices also need to be considered for physical therapy, which will be the next nursing epidemic.”
James Collins, Ph.D., MSME | Branch Chief, Analysis and Field Evaluations Branch, Division of Safety Research (DSR), National Institute for Occupational Safety and Health (NIOSH)
“Virtually impossible to predict when and if complete elimination of manual patient lifting will occur. Although there is a strong evidence base of research demonstrating that comprehensive safe patient handling and movement programs that include mechanical lifting equipment are highly effective for reducing the risk of injury to caregivers, only a portion of the industry has voluntarily implemented programs. Ten states currently have legislation mandating safe patient handling programs, but the goal of completely replacing manual patient lifting with mechanically assisted lifts will take many years to achieve. Unfortunately, to achieve this type of change is likely to be a 30-year process.”
Traci Galinsky, Ph.D. | CAPT, U.S. Public Health Service, National Institute for Occupational Safety and Health (NIOSH)
“Research has consistently demonstrated that body mechanics alone is not effective for preventing patient handling injuries. The proper use of patient handling devices is absolutely necessary for effective injury prevention. Nevertheless, even when equipment is used, some manual handling is typically required, for example, to help maneuver a patient into a lift sling or onto an airlift device. Body mechanics principles should be kept in mind during such tasks. I can’t predict the future, but it makes sense to expect that manual risk factors will continue to decrease with further innovations in safe patient handling technology.”
Gail Powell-Cope, Ph.D., ARNP, FAAN | Co-Director, Center of Innovation for Disability and Rehabilitation Research (CINDRR) at James A. Haley Veterans’ Hospital, Tampa, Florida
“Will it or should it? Many of us have been conducting safe patient handling research and program evaluation for over 15 years. If one goes by the widely held belief that it takes 17 years to translate research evidence into practice, then we have two years left to go. I am doubtful that we will reach that goal, but by 2024, I would like to see SPHM for all healthcare workers in all settings of care. The basic science evidence is clear that a health care worker cannot safely manually lift a load greater than 35 pounds, regardless of whether or not “good body mechanics” are used. Applied research is clear that SPHM programs reduce the risks of musculoskeletal injuries due to patient handling among healthcare workers. Emerging evidence is showing that SPHM increases the mobility of patients and reduces the hazards of immobility such as falls, pressure ulcers, and bowel and bladder dysfunction. SPHM should be a standard of care.”
Heather Monaghan, MHSc, RN | President/CEO, Visioning HealthCare Inc.
“It is important to understand that the research is definitive in that the use of body mechanics alone will not protect healthcare workers from musculoskeletal injury when lifting and moving patients. However, the principles of body mechanics should be used when using the equipment.”
Suzy Harrington, DNP, RN, MCHES | Chief Wellness Officer, Oklahoma State University
“There is no safe body mechanics. New technology is being developed every year, better meeting the safety needs of both patients and caregivers.”
Ninica Howard, MSc | Senior Occupational Health and Safety Researcher, SHARP Program at the Washington Department of Labor and Industries
“Mechanical lift equipment should replace manually handling patients whenever possible. Studies have found that “proper body mechanics” cannot overcome the physical stressors that are placed on the spine when moving or transferring patients. In one study, the author used the NIOSH lifting equation to calculate the maximum weight that could be safely lifted in a nursing care environment. Based on the body positioning of the care provider and several other factors, the maximum weight limit was calculated to be 35 lb.”
Nancy Hughes, MHA, BSN, RN | Board Member, American Association of Safe Patient Handling and Movement
“We certainly hope so. Body mechanics is proven not to be effective in handling patients while safe patient handling programs using equipment do reduce MSDs in health care workers. It is also safer for the patients. Body mechanics has its place, but not in moving people.”
Question #3: What obstacles do hospital administrators face when deciding whether or not to make the switch to machines and equipment to safeguard nursing staff?
Manon Labreche, PT, CEAS II | Injury Prevention Coordinator, Tampa General Hospital
“Senior management obstacles are usually financial in nature. Director and manager obstacles can include time for training, staff to maintain equipment, compliance issues, etc.”
William Marras, Ph.D., CPE | Executive Director & Scientific Director, Spine Research Institute at the Ohio State University
“Cost is the big obstacle. Overhead ceiling lifts are preferable but expensive. However, if the one considers the long-term cost savings (from reducing back injuries) instead of just the short-term equipment costs, there is no question that this is cost effective.”
Arun Garg, Ph.D., CPE, CSPHP | Director, Center for Ergonomics at the University of Wisconsin-Milwaukee
“Cost, training, lack of knowledge, reliance on equipment rather than program (i.e. systems approach). Many that have equipment produced no good results because of improper implementation.”
Guy Fragala, Ph.D., PE, CSP, CSPHP | Senior Advisor for Ergonomics, Patient Safety Center of Inquiry
“Initially, hospital administrators might see the cost of equipment as an obstacle. However, purchase and use of safe patient handling equipment has had a very good return on investment.”
Kermit Davis, Ph.D. | Graduate Program Director for Environmental and Occupational Hygiene Program, University of Cincinnati
“It is always driven by purchasing cost and compliance of the nurses using the equipment once purchased. While serving on the UCMC Safe Patient Handling Committee, I have seen firsthand several of these barriers. Culture is also a huge factor.”
James Collins, Ph.D., MSME | Branch Chief, Analysis and Field Evaluations Branch, Division of Safety Research (DSR), National Institute for Occupational Safety and Health (NIOSH)
“Low profit margins and fierce competition for budgets and resources.”
Traci Galinsky, Ph.D. | CAPT, U.S. Public Health Service, National Institute for Occupational Safety and Health (NIOSH)
“Implementing a safety program featuring ergonomic patient handling equipment and methods is a large, ongoing commitment. Success requires much more than simply purchasing equipment. Money, staff, time, and effort must be invested in order to start and sustain a program that provides frequent training, equipment maintenance, safety inspections, etc. Yet these obstacles are far outweighed by the benefits of safe patient handling programs. Research has shown that in effective programs, the financial investment is usually recovered within three to four years, followed by ongoing substantial savings associated with reduced injuries to staff and patients, reduced staff turnover, etc. And of course, injury and symptom prevention benefits not only the hospital staff and patients, but also their families, friends, and society as a whole.”
Gail Powell-Cope, Ph.D., ARNP, FAAN | Co-Director, Center of Innovation for Disability and Rehabilitation Research (CINDRR) at James A. Haley Veterans’ Hospital, Tampa, Florida
“I believe that hospital administrators are a main obstacle for full implementation of SPHM. If administrators prioritized SPHM for worker and patient safety and put resources (people, equipment, money) into it, managers and front line workers in the organization would follow suit. I would encourage administrators to learn the evidence, especially cost studies that have been conducted. The initial investment in SPHH will pay off over a 3-5 year period due to decreases in worker compensation costs and decreased staff turnover.”
Heather Monaghan, MHSc, RN | President/CEO, Visioning HealthCare Inc.
“Decision making is usually finance related. If a certain pot of money is put aside for workers compensation and injuries do not take costs above that, there is a perception that the financial cost of musculoskeletal injuries is not a big problem, as costs are “within budget.” Also, hospital budgets are often seen in silos. So while SPHM will impact many budgets including workers compensation, human resources, patient falls, length of stay, there is often a lack of either a lateral approach to the cost savings an SPHM program will bring, or a need for a fast fix return on investment that is not always seen. I believe every facility can afford an SPHM program. They just need to be creative about how it is funded, and draw money from a variety of budgets that will ultimately see the savings an SPHM will bring.”
Suzy Harrington, DNP, RN, MCHES | Chief Wellness Officer, Oklahoma State University
“Multi-levels based on the standards – lack of a safety culture and facility buy-in from the top down and bottom up, lack of technology, lack of available technology where it is needed, lack of a facility person dedicated to SPHM.”
Ninica Howard, MSc | Senior Occupational Health and Safety Researcher, SHARP Program at the Washington Department of Labor and Industries
“Ultimately, the decision by hospital administrators should always be to introduce lift and mobility equipment. Often, the cost of such equipment is presented as an obstacle but focused planning and implementation should not place a financial burden on the facility. Additionally, hospitals are continually introducing new things to improve the experience of the patient and those who visit the hospital. The focus is more commonly on the patient, and rightly so, than the staff who care for these patients. However, resources should be allocated towards the care staff to ensure that risks to their health are minimized. Budgets should be created to purchase equipment and the accessories necessary to continuous use of the equipment and patient handling equipment and/or supplies should remain a budgetary item to ensure that equipment is constantly updated.”
Nancy Hughes, MHA, BSN, RN | Board Member, American Association of Safe Patient Handling and Movement
“The cost of the initial equipment needed with multiple competing priorities. Yet, evidence has shown the return on investment for the equipment and the program, including reduction of injuries for healthcare workers.”
Question #4: How can hospitals be motivated to put the safety of their nurses first and implement the necessary changes?
Manon Labreche, PT, CEAS II | Injury Prevention Coordinator, Tampa General Hospital
“I feel that hospitals lack resources to be able to succeed with program implementations and sustaining them. Many do great at using vendors for initial training, but over time there is no follow-up and the program fails. Having a designated person in charge of such program has been proven effective.”
William Marras, Ph.D., CPE | Executive Director & Scientific Director, Spine Research Institute at the Ohio State University
“This requires a culture change. It is more than equipment. Attitudes and communication must change.”
Arun Garg, Ph.D., CPE, CSPHP | Director, Center for Ergonomics at the University of Wisconsin-Milwaukee
“Education, economic models.”
Guy Fragala, Ph.D., PE, CSP, CSPHP | Senior Advisor for Ergonomics, Patient Safety Center of Inquiry
“Hospitals should be very concerned with preserving their workforce. With projected nursing shortages and an aging workforce, it is very important that proper safe patient handling programs be implemented.”
Kermit Davis, Ph.D. | Graduate Program Director for Environmental and Occupational Hygiene Program, University of Cincinnati
“First question: why only hospitals? We also need to consider safe patient handling needs beyond hospitals as long-term care facilities and home health care have very unique handling problems. I think we need better documentation of the problem as many injured nurses are prone to leave the hospital setting or report them through medical coverage rather than reporting them as a compensable injury. We need to start thinking about how poor health of nurses impact patient safety and satisfaction. Money is the bottom line so we need to show that people who are trained to use the devices will have better compliance, better care for patients, and injuries are eliminated.”
James Collins, Ph.D., MSME | Branch Chief, Analysis and Field Evaluations Branch, Division of Safety Research (DSR), National Institute for Occupational Safety and Health (NIOSH)
“Motivating hospitals or other organizations to change culturally ingrained procedures requires a shift in philosophy and values. Many hospitals will take the initiative to be proactive in protecting their caregivers while other health care facilities will be slower to embrace change.”
Traci Galinsky, Ph.D. | CAPT, U.S. Public Health Service, National Institute for Occupational Safety and Health (NIOSH)
“Increased awareness of evidence-based research showing both the safety and the financial benefits of safe patient handling programs is needed. Information about safe patient handling research and related topics can be found at the NIOSH Safe Patient Handling Topic Page.”
Gail Powell-Cope, Ph.D., ARNP, FAAN | Co-Director, Center of Innovation for Disability and Rehabilitation Research (CINDRR) at James A. Haley Veterans’ Hospital, Tampa, Florida
“Some states have provided financial incentives to facilities, but I am not sure how well they have worked. Unfortunately, I am quite pessimistic of motivating hospitals to put the safety of nurses and nursing assistants first, although it is only logical that one needs a healthy workforce to be able to provide quality care for patients. An American Nurses Association survey from 2011 found that nurses are very concerned about the potential of disabling musculoskeletal injury, yet only 64% reported that patient lifting and transfer devices were readily available in their facilities. In part, because nursing is a women’s field and because nursing is viewed as a cost and not a revenue-generating contributor to the facility, nurses rank low in the pecking order in the world of health care. Nurses have not always been successful in persuading administrators to implement SPHM. I think it is very healthy for nurses to be speaking out to family, friends, and communities about the physical demands of their work. Everyone, including those in hospital administration, knows at least one nurse who has been injured due to patient care. Maybe when the issues are personal administrators will step up to the plate. Can you imagine us asking a dockworker to manually lift a 200-pound box? Nurses and nursing assistants lift and move patients weighing 200 pounds and more many times during one shift. I think the cost arguments help to persuade administrators, but ultimately I think the patient benefits of SPHM will be what motivate the healthcare industry to require SPHM programs. I want to emphasize though, that programs are more than just equipment. SPHM begins with equipment, but it takes leadership of the program, administrative support, interdisciplinary work, a system of initial and ongoing training (including release time to be trained), and active involvement of the front line staff. Also, schools of every discipline related to direct patient care need to make sure they are teaching the current, evidence-based practices for moving, transferring and lifting patients.”
Heather Monaghan, MHSc, RN | President/CEO, Visioning HealthCare Inc.
“The biggest motivator at the moment is how the implementation of SPHM affects patient outcomes, particularly in early mobility and falls reduction initiatives and the associated cost savings to the healthcare organization. A positive impact of this is nurses’ safety because they will be using technologies for lifting, repositioning, transferring and mobilizing their patients instead of manually handling their patients, thus reducing their injuries also. The biggest motivator for hospitals would be if The Joint Commission introduced SPHM as part of their patient safety goals as we are already seeing the body of evidence starting to grow on the patient benefits from SPHM.”
Suzy Harrington, DNP, RN, MCHES | Chief Wellness Officer, Oklahoma State University
“First, it is the right thing to do – it is not just for nurses and caregivers, it is for the safety of the patients as well. The ANA SPHM National Standards identify interprofessional standards for all areas of care. And, finally, the OSHA General Duty Clause pretty much sums it up: ‘General Duty Clause’ of the United States Occupational Safety and Health Act, 29 U.S.C 654, 5(a)1 ‘…each employer shall furnish to each of his employees, employment and a place of employment which are free from recognized hazards that are causing or are likely to cause death or serious physical harm to his employees.’”
Ninica Howard, MSc | Senior Occupational Health and Safety Researcher, SHARP Program at the Washington Department of Labor and Industries
“Hospitals should be motivated to make the necessary changes to not only protect the health of the nursing staff but also to protect the patient and to reduce the cost of patient handling related injuries. The cost of injuries to nursing staff (both in direct and indirect costs) far surpass the cost of introducing lift equipment into the environment. Additionally, the loss of experienced nursing staff to injury can deeply affect the quality of care that can be provided. The use of mechanical equipment can also help improve patient safety by reducing the potential for falls.”
Nancy Hughes, MHA, BSN, RN | Board Member, American Association of Safe Patient Handling and Movement
“Certainly the evidence of the effectiveness of the programs helps but doing the right thing for employees cannot be legislated. Regulations and accountability can only go so far depending on the cost of the fine, etc. but can help. Examples of the programs that are successful and those facilities taking the lead to educate their peers is very powerful particularly when they are in the same geographic area and there is competition for market share. Accrediting bodies such as the Joint Commission and also CMS can impact policy and practice. Tackling this issue is a multi-pronged approach.”
Question #5: What can be done to effect change at the federal level and ensure the safety of nurses across the nation? Does legislation need to be brought forward?
Manon Labreche, PT, CEAS II | Injury Prevention Coordinator, Tampa General Hospital
“Even with legislation, I don’t feel that will be enough. There has to be a commitment from the organization to institute the change and also a leader in the facility to address barriers as they come up. Hospitals change as well as patient population, therefore there must be a leader in the organization who can provide on-going education, address injuries, educate staff and managers, meet with vendors to look at latest technology, establish policies and procedures and modify them as needed, etc. I feel every hospital should have an injury prevention specialist to address injuries and develop programs that will make more of a difference than having legislation. JACHO would most likely be effective in instituting changes, as would Magnet more so than legislation.”
William Marras, Ph.D., CPE | Executive Director & Scientific Director, Spine Research Institute at the Ohio State University
“Unfortunately, in the absence of institutions doing the right thing, legislation becomes the only mechanism.”
Arun Garg, Ph.D., CPE, CSPHP | Director, Center for Ergonomics at the University of Wisconsin-Milwaukee
“Legislation will definitely help but need to be properly crafted.”
Guy Fragala, Ph.D., PE, CSP, CSPHP | Senior Advisor for Ergonomics, Patient Safety Center of Inquiry
“Healthcare reacts well to regulatory requirements and having safe patient handling legislation would be a big boost to moving efforts along. Previously, OSHA had enacted an Ergonomics Standard, which covered safe patient handling, but unfortunately, the standard was revoked through the Congressional Review Act. Efforts are in place for a new standard and only time will tell if and when it will be implemented. Beyond regulatory requirements, the healthcare industry must recognize the value of safe patient handling and mobility programs.”
Kermit Davis, Ph.D. | Graduate Program Director for Environmental and Occupational Hygiene Program, University of Cincinnati
“Yes. I almost just answered with the one-word answer as I think it is a resounding yes since many hospitals need to think big picture. Most of the time, lift assist devices are safer for patients too. Further, many facilities need to be encouraged to see the light. We need to have the big stick to make this happen widespread.”
James Collins, Ph.D., MSME | Branch Chief, Analysis and Field Evaluations Branch, Division of Safety Research (DSR), National Institute for Occupational Safety and Health (NIOSH)
“As a federal government scientist, I am not allowed to lobby for legislation or promote policies. A federal bill was brought forward previously but was not passed into law. If safe patient handling legislation and policy follows the trend of needlestick and sharps legislation, after approximately 15 states passed laws, it created sufficient momentum for federal legislation to follow.”
Traci Galinsky, Ph.D. | CAPT, U.S. Public Health Service, National Institute for Occupational Safety and Health (NIOSH)
“As noted on the NIOSH topic page, no federal safe patient handling law has yet been enacted. The most recently introduced federal bill is the Nurse and Health Care Worker Protection Act of 2013 (H.R. 2480). We hope that studies by NIOSH and other researchers showing the benefits of Safe Patient Handling programs will be used by policy makers to inform their legislative decisions.”
Gail Powell-Cope, Ph.D., ARNP, FAAN | Co-Director, Center of Innovation for Disability and Rehabilitation Research (CINDRR) at James A. Haley Veterans’ Hospital, Tampa, Florida
“I used to be on the fence about whether or not we needed federal legislation, but not anymore. I just don’t think health care will change without it. Again, nurses and all healthcare workers who provide patient care need to raise their voices to their representatives and senators. Let them know about the extent of the problem and the solutions. Work with the American Nurses Association, the American Physical Therapy Association and other professional organizations who have provided leadership in supporting SPHM legislation. SPHM is not just for nurses. It is for all healthcare workers in direct patient care including but not limited to physical therapists and physical therapy assistants, occupational therapists, technicians in diagnostic areas, medical technicians, emergency medical technicians, and paramedics.”
Heather Monaghan, MHSc, RN | President/CEO, Visioning HealthCare Inc.
“I think we need to build up the support for SPHM through organizations such as NIOSH, and associations such as the ANA, AASPHM and ASPHP, and contact our state representatives to make them aware of the injuries that are occurring to caregivers when moving and handling patients. The recent radio series on SPHM by NPR’s investigation unit has been very powerful. We need more media exposure so the public understands the issue – many are not even aware.”
Suzy Harrington, DNP, RN, MCHES | Chief Wellness Officer, Oklahoma State University
“Absolutely! Legislation was drafted based on the ANA SPHM National Standards. Talk with state and federal political leaders! A fabulous NPR series just came out in February.”
Ninica Howard, MSc | Senior Occupational Health and Safety Researcher, SHARP Program at the Washington Department of Labor and Industries
“The American Nurses Association has long campaigned for actions to reduce patient handling related injuries to care staff. A nationally coordinated effort by labor representatives and unions may help push this topic to the forefront. Legislation does need to be brought forward in order to establish the minimum standard by which organizations must adhere to. The implementation of a safe patient handling and mobility environment, as well as the support for change, can vary greatly by facility and organization.”
Nancy Hughes, MHA, BSN, RN | Board Member, American Association of Safe Patient Handling and Movement
“Federal agencies such as OSHA can help to set standards and give health care workers some advocacy. Federal funding including grants can help as well. Professional associations can help to inform federally. Legislation can help as it did in needlestick safety. Legislating for funding can also assist the hospitals to strengthen their safe lifting programs. If facilities are not held accountable, it does nothing more. Again, professional associations can help to inform legislators at the state and federal level.”



No Comment